Managing food sensitivities, intolerances, and gut health is crucial for those with chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME). By identifying and eliminating problematic foods, healing the gut, and supporting a balanced microbiome, you can potentially reduce fatigue, brain fog, digestive issues, and other CFS/ME symptoms.
Related video from YouTube
Key Points
- Food sensitivities and intolerances, unlike allergies, do not involve the immune system but can still cause unpleasant symptoms like digestive issues, fatigue, brain fog, and joint pain.
- There is a strong link between gut health and CFS/ME, with gut dysbiosis and leaky gut contributing to inflammation and worsening symptoms.
- Strategies to manage food issues and improve gut health include:
- Elimination diets and food sensitivity testing to identify trigger foods
- Gut-healing protocols like probiotics, prebiotics, and digestive enzymes
- Lifestyle changes like stress management, exercise, and sleep hygiene
Common Problematic Foods in CFS/ME
- Alcohol
- Caffeine and stimulants
- Sweeteners (sugar, corn syrup, fructose, aspartame, saccharin)
- Food additives (MSG, preservatives, artificial colors/flavors)
- Dairy products
- Gluten/wheat
- Nightshade vegetables (tomatoes, potatoes, eggplants)
Gut Health Strategies
| Strategy | Potential Benefits |
|---|---|
| Probiotic Foods | Restore gut microbiome balance, improve digestion |
| Prebiotic Fiber | Feed beneficial gut bacteria, promote diversity |
| Varied Plant-Based Diet | Provide different types of nourishing fiber |
| L-Glutamine | Rebuild and strengthen gut lining |
| Bone Broth | Rich in collagen and amino acids for gut healing |
| Omega-3 Fatty Acids | Reduce inflammation |
Getting Professional Help
Consult healthcare professionals like registered dietitians or functional medicine practitioners for personalized guidance on managing food sensitivities, intolerances, and gut health in relation to CFS/ME. They can help with identifying triggers, developing dietary plans, and addressing any underlying conditions or nutrient deficiencies.
Understanding Food Issues
Food Allergies vs. Sensitivities vs. Intolerances
| Condition | Immune System Involved? | Symptom Onset | Severity |
|---|---|---|---|
| Food Allergy | Yes | Rapid | Can be life-threatening |
| Food Sensitivity | No | Delayed | Not life-threatening |
| Food Intolerance | No | Delayed | Not life-threatening |
Food allergies trigger an immune system response, even with small amounts of the food. Symptoms appear quickly and can be severe, even life-threatening in some cases.
Food sensitivities and intolerances, on the other hand, do not involve the immune system. Symptoms appear gradually after consuming the problematic food and are generally less severe.
Common Symptoms
Common symptoms of food sensitivities and intolerances include:
- Digestive issues:
- Bloating
- Gas
- Diarrhea
- Constipation
- Fatigue
- Brain fog and difficulty concentrating
- Headaches
- Joint pain
- Skin problems like rashes and eczema
These symptoms can overlap with and worsen CFS/ME symptoms, making it hard to distinguish between the two conditions.
Impact on CFS/ME and Health
Food sensitivities and intolerances can significantly impact the health and well-being of individuals with CFS/ME. They can contribute to:
- Increased fatigue and post-exertional malaise
- Cognitive impairments, including brain fog and difficulty concentrating
- Worsening of gastrointestinal symptoms, such as bloating and diarrhea
- Increased inflammation and oxidative stress
- Exacerbation of other CFS/ME symptoms, like muscle pain and headaches
Identifying and managing food sensitivities and intolerances is crucial for reducing symptom severity and improving overall health in CFS/ME patients.
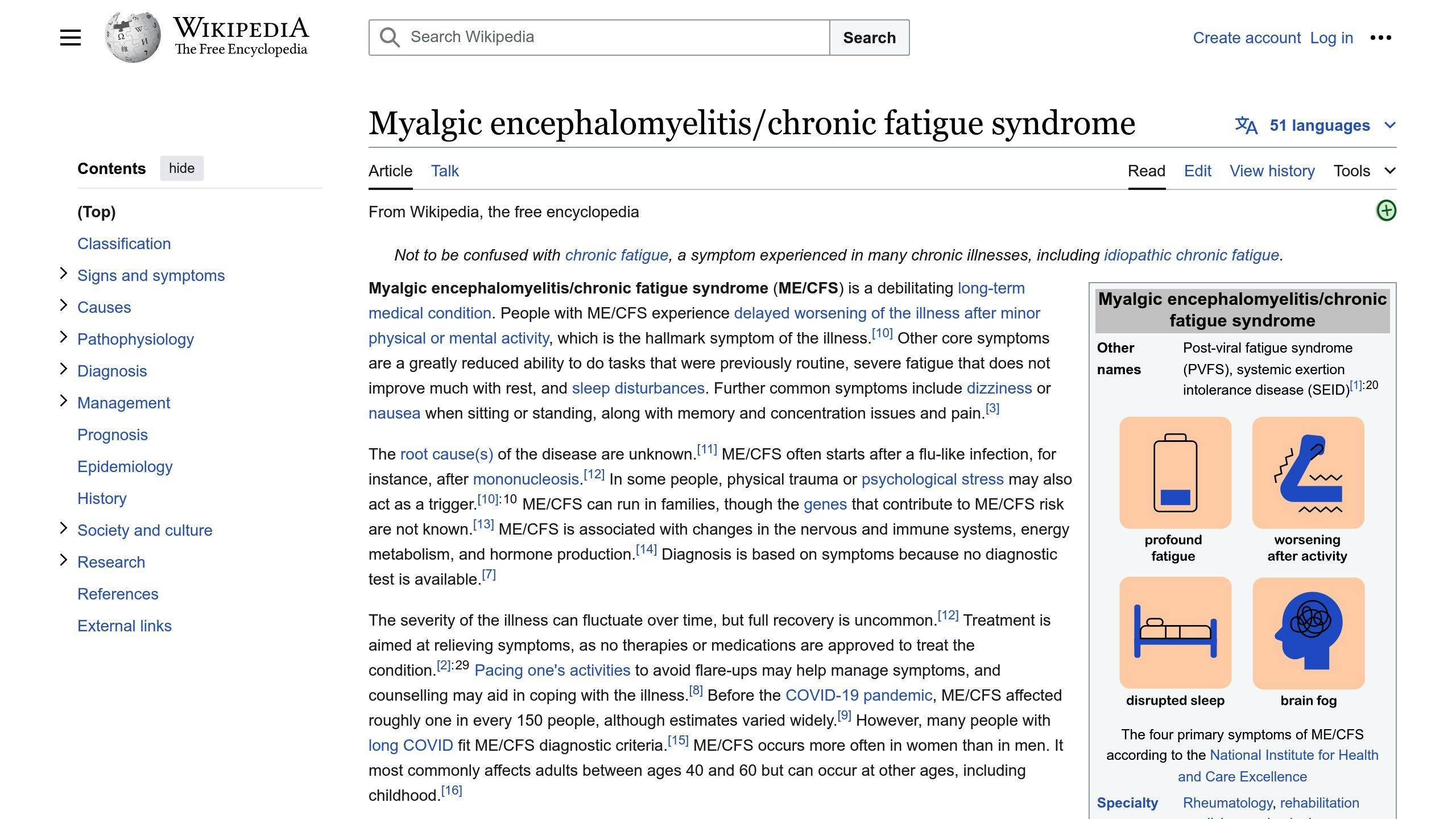
Gut Health and CFS/ME
Gut-Brain Connection
The gut and brain have a close two-way communication link called the gut-brain axis. This connection allows the gut microbiome (gut bacteria) and gut functions to impact brain health, and vice versa. In CFS/ME, problems with gut health can contribute to brain fog, trouble concentrating, fatigue, and other neurological issues.
Common Gut Issues
Two common gut problems in CFS/ME patients are:
- Gut Dysbiosis: An imbalance in the gut microbiome.
- Leaky Gut: A condition where the intestinal barrier becomes permeable, allowing harmful substances like bacteria, toxins, and partially digested food particles to enter the bloodstream.
These issues can trigger an immune response and widespread inflammation, potentially worsening food sensitivities and intolerances.
Why Gut Health Matters
Maintaining a healthy gut is crucial for managing CFS/ME symptoms and improving overall well-being. A balanced gut microbiome supports:
- Proper digestion
- Nutrient absorption
- Immune function
It also helps regulate inflammation levels and prevents leaky gut. By addressing gut health, individuals with CFS/ME may experience:
| Potential Benefits |
|---|
| Reduced food sensitivities |
| Improved energy levels |
| Better cognitive function |
| Alleviated gastrointestinal issues |
sbb-itb-cf04d29
Finding Problem Foods
Elimination Diet
An elimination diet helps find foods that may cause issues. You remove certain foods from your diet for 2-4 weeks, then slowly add them back one by one. This lets you see which foods trigger symptoms.
To do an elimination diet:
-
Keep a Food Diary: Write down everything you eat and any symptoms you have. This helps spot problem foods.
-
Eliminate Potential Triggers: Stop eating common allergens like gluten, dairy, soy, eggs, nuts, and processed foods. Stick to simple, whole foods.
-
Reintroduce Foods Slowly: After 2-4 weeks, add back one food group at a time. Wait a few days before adding the next group.
-
Watch for Reactions: Note any changes in fatigue, brain fog, digestion, joint pain, etc. Record them in your food diary.
-
Get Professional Help: Work with a dietitian or doctor to ensure you follow the diet properly and get proper nutrition.
Food Sensitivity Tests
Food sensitivity tests can also identify problem foods. These tests look for reactions to certain foods.
| Test | How It Works | Pros | Cons |
|---|---|---|---|
| IgG Blood Test | Measures antibody levels for food sensitivities | Shows many sensitivities | May have false results, expensive |
| ALCAT Test | Checks for cellular reactions to foods | Finds non-IgG sensitivities | Less proven, may miss some |
| Skin Prick Test | Tests for allergic reactions under the skin | Widely available, affordable | Only finds allergies, not intolerances |
Comparing Tests
| Test | Advantages | Drawbacks |
|---|---|---|
| Elimination Diet | Accurate, personalized | Time-consuming, strict |
| Blood Tests | Quick results | Potential false results, costly |
| ALCAT Test | Detects cellular reactions | Less validated, incomplete |
Managing Food Issues
Diet Changes
1. Elimination Diet: This diet helps find foods that cause issues. You stop eating common trigger foods like gluten, dairy, soy, eggs, and processed items for 2-4 weeks. Then, you slowly add them back one by one while noting any symptoms. This shows which foods are problematic for you.
2. Food Swaps: Once you know which foods trigger reactions, find suitable replacements. For lactose issues, try lactose-free milk or dairy alternatives. For gluten sensitivity, choose gluten-free bread, pasta, and baked goods. Read labels carefully and try new ingredients.
3. Rotation Diet: If you can handle some foods in moderation, try a rotation diet. Eat the food, then avoid it for 4-7 days before eating it again. This rotation can prevent reactions from building up over time.
Gut Healing
1. Probiotics: These "good" bacteria help restore a healthy gut and improve digestion. Eat probiotic-rich foods like yogurt, kefir, sauerkraut, or take a probiotic supplement.
2. Prebiotics: Prebiotics are fibers that feed the beneficial gut bacteria. Good sources include onions, garlic, bananas, and whole grains. Prebiotic supplements can also help.
3. Digestive Enzymes: Enzyme supplements can aid in breaking down foods and reduce digestive discomfort. Look for enzymes like lactase for lactose issues or alpha-galactosidase for gas and bloating.
Lifestyle Changes
| Change | Benefit |
|---|---|
| Stress Management | Chronic stress can worsen gut issues and food sensitivities. Practice relaxation techniques like meditation, yoga, deep breathing, or enjoyable activities. |
| Exercise | Regular moderate exercise can improve gut health by promoting better digestion, reducing inflammation, and supporting a diverse gut microbiome. |
| Sleep Hygiene | Getting enough quality sleep is crucial for gut healing and overall well-being. Aim for 7-9 hours per night and establish a consistent sleep routine. |
Improving Gut Health
Balanced Gut Microbiome
To support a healthy gut microbiome, consider these options:
- Probiotic Foods: Eat fermented foods like yogurt, kefir, sauerkraut, kimchi, and kombucha. They contain live beneficial bacteria that aid gut health.
- Prebiotic Fiber: Prebiotics feed the good gut bacteria. Increase your intake of prebiotic-rich foods like onions, garlic, asparagus, bananas, and whole grains.
- Varied Diet: Eating a wide range of plant-based foods provides different types of fiber that nourish the gut microbiome.
- Probiotic Supplements: Consider a high-quality probiotic supplement with diverse strains like Lactobacillus and Bifidobacterium.
Healing Leaky Gut
To repair a leaky gut and reduce inflammation, try:
- L-Glutamine: This amino acid helps rebuild and strengthen the gut lining.
- Bone Broth: Rich in collagen and amino acids that promote gut healing.
- Aloe Vera: Known for soothing the gut lining and reducing inflammation.
- Turmeric: Curcumin, the active compound in turmeric, has anti-inflammatory effects.
- Omega-3 Fatty Acids: Found in fatty fish, walnuts, and flaxseeds, they help reduce inflammation.
Gut Healing Approaches
| Approach | Key Components | Potential Benefits | Potential Drawbacks |
|---|---|---|---|
| Probiotic Therapy | Bifidobacteria, Lactobacillus | May reduce inflammation, improve gut flora | Initial digestive discomfort possible |
| Dietary Changes | High-fiber foods, low fermentable foods | Supports gut health, may reduce symptoms | Requires dietary adjustments, learning curve |
| Herbal Supplements | Glutamine, licorice root | May repair gut lining, reduce inflammation | Possible side effects, medication interactions |
| Elimination Diet | Removes common trigger foods | Identifies food sensitivities | Restrictive, challenging long-term |
| Anti-Inflammatory Diet | Emphasizes whole, nutrient-dense foods | May reduce inflammation, promote healing | Requires lifestyle changes |
Tracking Your Progress
Keeping a Food and Symptom Diary
Maintaining a detailed food and symptom diary is key to identifying potential food triggers and monitoring your progress. Record everything you eat and drink, along with any symptoms you experience, their severity, and the time they occur. Be specific in describing the foods and symptoms. This diary will help you spot patterns and connections between certain foods and your body’s reactions.
Reintroducing Foods Step-by-Step
After an elimination phase, reintroduce foods one by one to determine your tolerance levels:
1. Reintroduce one food
Eat the eliminated food in increasing amounts throughout the day, starting with a small portion at each meal.
2. Monitor for 2-3 days
Observe for any reactions or symptoms over the next 2-3 days. Record your observations in your food and symptom diary.
3. Eliminate and move on
If you experience symptoms, eliminate that food again. If not, you can likely tolerate it. Then, move on to reintroducing the next food.
4. Repeat the process
Cycle through reintroducing each eliminated food, one by one, following the same process.
Adjusting Your Approach
Your approach should be flexible and tailored to your individual needs and progress. Regularly review your food and symptom diary, and adjust your diet and strategies accordingly:
| Action | Description |
|---|---|
| Identify patterns | Look for patterns in your symptoms and potential food triggers. |
| Modify your diet | Based on your findings, modify your diet by eliminating or reducing problematic foods and incorporating well-tolerated ones. |
| Seek professional guidance | If you struggle to identify triggers or manage symptoms, consider consulting a healthcare professional or dietitian for personalized guidance. |
| Be patient | Healing the gut and finding the right dietary approach takes time. Be patient and persistent, and don’t hesitate to adjust your approach as needed. |
Getting Professional Help
When to Seek Assistance
It’s wise to consult healthcare experts when dealing with food sensitivities and chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME). Seek professional help if you experience:
- Severe or persistent symptoms like digestive issues, migraines, or muscle weakness that greatly impact your daily life.
- Difficulty identifying problematic foods or managing symptoms through diet changes alone.
- Concerns about nutritional deficiencies or imbalances due to restrictive diets.
- Complications or other health conditions that require medical attention.
Personalized Guidance
Working with healthcare professionals can provide personalized guidance tailored to your specific needs and situation. They can:
- Evaluate your medical history, symptoms, and dietary habits.
- Recommend appropriate food sensitivity tests or elimination diets.
- Develop a plan for dietary modifications and gut healing strategies.
- Monitor your progress and adjust the plan as needed.
- Provide guidance on supplements and lifestyle changes.
- Address any underlying conditions or nutrient deficiencies.
Common Challenges and Considerations
Managing food sensitivities and gut health in CFS/ME can be challenging. Here are some common challenges and considerations:
| Challenge | Consideration |
|---|---|
| Identifying triggers | Keep a detailed food and symptom diary to pinpoint problematic foods. |
| Restrictive diets | Work closely with a professional to ensure a balanced and nutritious diet. |
| Gut healing | Be patient, as healing the gut and restoring balance takes time. |
| Lifestyle factors | Address stress, sleep, and exercise to support gut health. |
| Coexisting conditions | Manage any other conditions that may impact gut health and food sensitivities. |
| Emotional support | Seek support from loved ones or support groups to cope with dietary changes and symptoms. |
Conclusion
Managing food sensitivities, intolerances, and gut health is vital for those with chronic fatigue syndrome/myalgic encephalomyelitis (CFS/ME). By finding problematic foods and addressing gut issues, you may ease symptoms and improve overall well-being.
The path to better gut health and reduced food sensitivities can be challenging, but patience and persistence are key. Work closely with healthcare professionals to develop a personalized plan, including an elimination diet, gut-healing strategies, and lifestyle changes. Remember, healing the gut and restoring balance takes time, so stay consistent and celebrate small wins along the way.
If you struggle to manage food sensitivities or gut health issues alone, don’t hesitate to seek professional guidance. A healthcare team can provide valuable support, monitor your progress, and adjust your plan as needed.
Ultimately, improving gut health and addressing food sensitivities can significantly impact your overall health and quality of life with CFS/ME. Stay committed to the process, and don’t lose hope – with the right approach and support, you can take steps towards better gut health and symptom management.
For further reading and support, consider exploring reputable online resources, joining support groups, or consulting with organizations dedicated to CFS/ME and gut health.
FAQs
Can Food Intolerance Cause Chronic Fatigue?
Yes, food intolerances and sensitivities can contribute to chronic fatigue in the following ways:
-
Immune Response: When the body perceives a food as a threat due to intolerance, it triggers an immune response to fight it off. This process uses up energy reserves, leading to fatigue.
-
Gut Inflammation: Food sensitivities can cause inflammation in the gut, impairing nutrient absorption and leaving you feeling drained.
-
Secondary Symptoms: Fatigue may arise from dealing with other symptoms like irritable bowel syndrome (IBS), cramps, migraines, etc., caused by food intolerances.
What Food Sensitivities Are Common in Myalgic Encephalomyelitis?
Many individuals with ME/CFS (myalgic encephalomyelitis/chronic fatigue syndrome) experience sensitivities to:
| Common Food Sensitivities in ME/CFS |
|---|
| Alcohol |
| Caffeine and stimulants |
| Sweeteners (sugar, corn syrup, fructose, aspartame, saccharin) |
| Food additives (MSG, preservatives, artificial colors/flavors) |
| Dairy products |
| Gluten/wheat |
| Nightshade vegetables (tomatoes, potatoes, eggplants) |
However, food sensitivities can vary greatly from person to person. An elimination diet and careful reintroduction of foods can help identify problematic items for each individual.
Related posts
- 10 Nutrition Tips to Manage Chronic Fatigue Syndrome
- 10 Key Nutrients for CFS/ME Management
- Probiotics Improve Cognitive Function in ME/CFS
- Macronutrient Balance for CFS/ME Energy





Leave a Reply