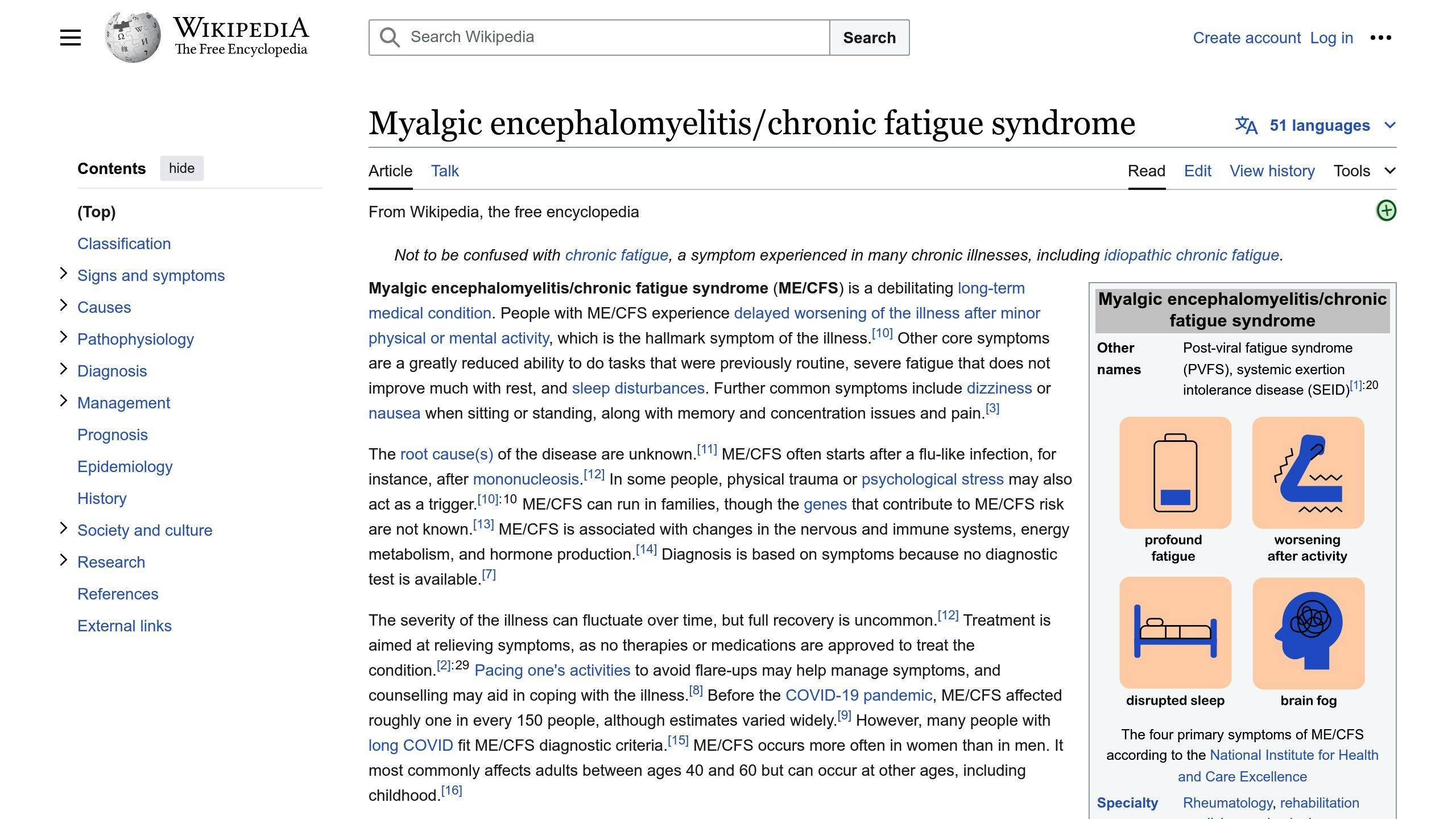
Chronic Fatigue Syndrome (CFS/ME) is a complex condition characterized by severe, long-lasting fatigue and various symptoms like brain fog, sleep disturbances, and digestive issues. Recent research has revealed a potential link between gut health and CFS/ME, with individuals suffering from the condition often exhibiting imbalances in their gut microbiome.
Key Findings:
- CFS/ME patients tend to have lower levels of beneficial gut bacteria like Faecalibacterium prausnitzii and Eubacterium rectale, which produce anti-inflammatory compounds like butyrate.
- Higher levels of bacteria linked to inflammation and autoimmune diseases are commonly found in CFS/ME patients.
- Reduced microbial diversity and an overall imbalance in the gut microbiome composition are observed in those with CFS/ME.
Gut microbiome testing can provide valuable insights into these imbalances and guide personalized treatment plans, such as dietary changes, probiotic supplementation, and therapies to restore gut health.
Testing Options:
| Test Type | Description |
|---|---|
| Stool Tests | Analyze the types and amounts of gut bacteria, as well as substances they produce. |
| Breath Tests | Detect specific gut conditions like Small Intestinal Bacterial Overgrowth (SIBO). |
| Blood Tests | Measure markers of inflammation and immune function related to gut health. |
When to Consider Testing:
- You have CFS/ME and experience chronic digestive issues like diarrhea, constipation, bloating, or food intolerances.
- You recently had an illness or infection that preceded your CFS/ME symptoms.
- You’ve taken antibiotics recently or frequently.
- You have an unhealthy diet, high stress levels, or lack physical activity.
- You have a family history of CFS/ME, autoimmune disorders, or gut-related conditions.
If you suspect gut issues may be contributing to your CFS/ME symptoms, discuss the potential benefits of gut microbiome testing with your healthcare provider. They can help determine the most appropriate testing approach and develop a tailored treatment plan based on your results.
Related video from YouTube
Gut Microbiome Tests
There are various tests to examine the gut microbiome in people with Chronic Fatigue Syndrome (CFS/ME). These tests provide insights into the types and amounts of gut bacteria, as well as specific bacterial strains and substances they produce.
Stool Tests
Stool tests are the most common way to analyze the gut microbiome. These tests involve collecting a stool sample, which is then analyzed using different methods:
- Metagenomics Sequencing: This technique identifies the DNA of all the microorganisms in the stool sample, showing the types and amounts of gut bacteria present.
- Polymerase Chain Reaction (PCR): PCR detects and measures specific bacterial strains or groups in the stool sample.
- Metabolomics: This method looks at the substances produced by gut bacteria, which can show how they may affect health.
Stool tests can reveal information about the levels of good and potentially harmful bacteria, as well as the overall diversity and balance of the gut microbiome.
Breath Tests
Breath tests are non-invasive methods used to check for specific gut conditions, such as Small Intestinal Bacterial Overgrowth (SIBO). These tests involve drinking a specific substance, like lactulose or glucose, and measuring the levels of gases (e.g., hydrogen, methane) produced by gut bacteria in the exhaled breath.
While breath tests do not provide a complete analysis of the gut microbiome, they can help detect imbalances in certain bacterial populations or identify conditions like SIBO, which may contribute to CFS/ME symptoms.
Blood Tests
Blood tests can measure markers of inflammation and immune function, which may be affected by the gut microbiome. These tests can check levels of inflammatory substances, antibodies, and other markers that may be elevated in people with CFS/ME.
While blood tests do not directly analyze the gut microbiome, they can provide insights into the body-wide effects of gut imbalances and help identify potential links between gut health and CFS/ME symptoms.
| Test Type | Advantages | Disadvantages | Best For |
|---|---|---|---|
| Stool Tests | Shows types and amounts of gut bacteria | Collecting sample can be uncomfortable | Getting a complete picture of the gut microbiome |
| Breath Tests | Non-invasive | Limited to certain conditions (e.g., SIBO) | Detecting specific gut conditions like SIBO |
| Blood Tests | Shows inflammation and immune function | Less direct information about the gut | Assessing inflammation and immune markers related to gut health |
The choice of test(s) will depend on the specific goals and concerns of the individual with CFS/ME, as well as the recommendations of their healthcare provider.
Understanding Test Results
Key Bacterial Strains
Some bacterial strains are often found in lower levels in people with Chronic Fatigue Syndrome (CFS/ME), including:
-
Faecalibacterium prausnitzii: This bacterium produces butyrate, a fatty acid that helps keep the gut healthy. Lower levels of F. prausnitzii have been linked to more severe fatigue symptoms in CFS/ME patients.
-
Eubacterium rectale: Another butyrate-producing bacterium that is typically reduced in CFS/ME patients. Butyrate helps maintain the gut lining and regulates immune function.
-
Acetate-producing bacteria: Certain bacteria that produce acetate, another fatty acid important for gut health and metabolism, have also been found to be less abundant in CFS/ME patients.
Microbial Diversity
Studies consistently show that individuals with CFS/ME tend to have lower overall diversity in their gut microbiome compared to healthy individuals. This reduced diversity can indicate an imbalanced or dysbiotic gut environment, which may contribute to the development or worsening of CFS/ME symptoms.
Higher microbial diversity is generally associated with better gut health, as a diverse microbiome is better equipped to perform various metabolic functions and maintain a balanced immune response.
Metabolite Levels
Gut microbiome tests may also measure the levels of various metabolites produced by gut bacteria. Some key metabolites that may be altered in CFS/ME patients include:
-
Butyrate: As mentioned earlier, butyrate is a fatty acid produced by certain bacteria like F. prausnitzii and E. rectale. Lower levels of butyrate have been associated with various health conditions, including CFS/ME.
-
Tryptophan metabolites: Tryptophan is an amino acid that is metabolized by gut bacteria into various compounds, some of which can influence immune function and neurotransmitter production. Imbalances in tryptophan metabolism have been observed in CFS/ME patients.
-
Inflammatory markers: Gut microbiome tests may also measure the levels of inflammatory markers, such as lipopolysaccharides (LPS) or cytokines, which can indicate the presence of gut inflammation or immune dysregulation.
Step-by-Step Guide
When interpreting gut microbiome test results, consider the following step-by-step approach:
-
Assess bacterial diversity: Look at the overall diversity of the gut microbiome, as lower diversity is often associated with dysbiosis and potential health issues.
-
Identify key bacterial strains: Check the levels of important bacterial strains like F. prausnitzii, E. rectale, and acetate-producing bacteria. Low levels of these bacteria may indicate an imbalance in the gut microbiome.
-
Evaluate metabolite levels: Examine the levels of butyrate, tryptophan metabolites, and inflammatory markers. Deviations from normal ranges may suggest gut dysbiosis or immune dysregulation.
-
Consider symptom severity: Correlate the test results with the severity of your CFS/ME symptoms. For example, lower levels of F. prausnitzii have been associated with more severe fatigue symptoms.
-
Consult with a healthcare professional: Discuss the test results with a qualified healthcare provider who can help interpret the findings and recommend appropriate treatment or lifestyle interventions based on your specific situation.
Getting Ready for Testing
Diet Prep
For about a week before the test, stick to your normal eating habits. This helps ensure the results show your typical gut bacteria. Here are some tips:
- Avoid antibiotics: Don’t take antibiotics for at least 4-6 weeks before testing, as they can disrupt your gut bacteria.
- Stop probiotics: Don’t take probiotic supplements for 2 weeks before the test, as they can temporarily change your gut bacteria.
- Eat as usual: Follow your regular diet and don’t make big changes in the week before testing.
- Eat more fiber: Eating fiber-rich foods can promote a healthy, diverse gut microbiome, which may help with the test results.
Medications
Let your doctor know about any medications you’re taking, as some can affect the test results. These include:
- Antibiotics: As mentioned, antibiotics can significantly impact your gut bacteria.
- Acid reflux meds: Proton pump inhibitors (PPIs) for acid reflux or stomach ulcers can change your gut bacteria by reducing stomach acid.
- Pain relievers: Long-term use of non-steroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or naproxen may affect your gut bacteria and cause inflammation.
Sample Collection
Proper sample collection is key for accurate results. Follow these steps:
- Use the kit: The testing kit will have all the supplies you need, like a sterile container and instructions.
- Fresh sample: Collect a fresh stool sample, as exposure to air or contamination can affect the results.
- Handle with care: Follow any instructions for storing, keeping cool, and transporting the sample to keep it viable for testing.
- Provide details: Fill out any forms or questionnaires accurately, including your diet, medications, and medical history.
| Preparation | What to Do |
|---|---|
| Diet | Eat your normal diet, avoid antibiotics and probiotics, increase fiber intake |
| Medications | Inform your doctor about any medications you’re taking, especially antibiotics, acid reflux meds, and NSAIDs |
| Sample Collection | Use the provided kit, collect a fresh sample, handle it carefully, and provide accurate information |
sbb-itb-cf04d29
When to Test
Recognizing Symptoms
You may want to consider gut microbiome testing if you have chronic fatigue syndrome (CFS/ME) and experience ongoing gut issues like:
- Chronic diarrhea or constipation
- Bloating and stomach discomfort
- Food intolerances or sensitivities
- Unexplained nutrient deficiencies
If these gut symptoms occur alongside CFS/ME symptoms like fatigue, brain fog, and feeling worse after activity, it could indicate an imbalance in your gut bacteria.
Personal Health Factors
Beyond symptoms, certain personal health factors may also suggest the need for gut microbiome testing:
| Personal Factor | Reason for Testing |
|---|---|
| Recent illness or infection | Many CFS/ME cases start after a viral or bacterial infection, which can disrupt gut bacteria. |
| Antibiotic use | Antibiotics can significantly alter the gut microbiome. |
| Unhealthy diet and lifestyle | Poor diet, high stress, and lack of exercise can contribute to gut imbalances. |
| Family history | A family history of CFS/ME, autoimmune disorders, or gut-related conditions may increase the relevance of testing. |
Decision Guide
Consider gut microbiome testing if:
1. You have CFS/ME and experience:
- Chronic diarrhea, constipation, bloating, or food intolerances
2. You recently had an illness or infection that preceded your CFS/ME symptoms.
3. You’ve taken antibiotics recently or frequently.
4. You have an unhealthy diet, high stress levels, or lack physical activity.
5. You have a family history of CFS/ME, autoimmune disorders, or gut-related conditions.
If any of these apply to you, discuss the potential benefits of gut microbiome testing with your healthcare provider. They can help determine if testing is appropriate based on your specific circumstances and symptoms.
Integrating Test Results
Diet Changes
Based on your gut microbiome test results, your doctor may suggest changes to your diet to help restore balance and improve gut health. Common tips include:
-
Eat more fiber: Fiber feeds good gut bacteria like Faecalibacterium prausnitzii and Roseburia spp. Good sources are fruits, veggies, whole grains, nuts, and seeds.
-
Cut back on processed foods: These lack fiber and can feed harmful gut bacteria. Focus on whole, minimally processed foods.
-
Limit trigger foods: Your test may show intolerances or sensitivities to certain foods like dairy, gluten, or FODMAPs. Avoiding these temporarily can reduce gut inflammation.
-
Try fermented foods: Foods like yogurt, kefir, sauerkraut, and kimchi provide probiotics to support a healthy microbiome.
Probiotics and Prebiotics
Your doctor may recommend probiotic supplements with strains like Lactobacillus and Bifidobacterium to replenish good gut bacteria depleted in CFS/ME. Prebiotic fiber supplements like inulin can also help feed and grow these good bacteria.
Some probiotics like Faecalibacterium prausnitzii have shown promise in early research for easing CFS/ME symptoms by producing anti-inflammatory compounds like butyrate. However, more research is still needed.
Other Treatments
In severe cases of gut dysbiosis, your doctor may consider more intensive treatments like:
| Treatment | Description |
|---|---|
| Fecal microbiota transplantation (FMT) | Transferring healthy donor stool to restore a balanced gut microbiome. |
| Antibiotic therapy | Short-term antibiotics may help eliminate harmful gut bacteria before reintroducing good strains. |
| Herbal antimicrobials | Natural compounds like berberine can selectively target and eliminate problematic gut microbes. |
Working with Doctors
It’s crucial to work closely with your doctor and a team of specialists when interpreting gut microbiome test results and planning treatment. They can:
1. Evaluate your overall health and CFS/ME symptoms.
2. Determine appropriate dietary, probiotic, or other interventions.
3. Monitor your progress and adjust the treatment plan as needed.
4. Coordinate care from gastroenterologists, nutritionists, and other experts.
Test Limitations
Test Accuracy
Gut microbiome tests offer insights, but they have limits and potential inaccuracies. These tests analyze the gut microbiome at a single point in time, but the gut microbiome changes due to various factors. Different testing methods and labs may yield slightly different results.
Factors Affecting Results
Several factors can impact the accuracy and interpretation of gut microbiome test results:
| Factor | Impact |
|---|---|
| Diet | What you eat significantly affects your gut microbiome. Dietary changes before testing may skew results. |
| Medications | Antibiotics, probiotics, and other medications can temporarily alter the gut microbiome, leading to inaccurate results. |
| Lifestyle | Stress, sleep, exercise, and environmental exposures can affect the gut microbiome. |
| Sample Handling | Improper sample collection, storage, or transportation can compromise the sample and result accuracy. |
Professional Guidance
Given the gut microbiome’s complexity and potential confounding factors, work with qualified healthcare professionals when interpreting test results and making treatment decisions. Experienced practitioners can:
1. Evaluate your overall health, medical history, and CFS/ME symptoms in the context of the test results.
2. Identify potential factors that may have influenced the test results.
3. Recommend appropriate dietary, probiotic, or other interventions based on the test results and your specific needs.
4. Monitor your progress and adjust the treatment plan as needed.
5. Coordinate care with specialists like gastroenterologists, nutritionists, and immunologists for a comprehensive approach.
Summary
Gut Microbiome Testing for Chronic Fatigue Syndrome
Gut microbiome testing offers insights into gut health for those with chronic fatigue syndrome (CFS/ME). These tests analyze the types and amounts of gut bacteria, as well as substances they produce.
Key Findings
- CFS/ME patients often have:
- Lower levels of good bacteria like Faecalibacterium prausnitzii and Eubacterium rectale
- Higher levels of bacteria linked to inflammation and autoimmune diseases
- Reduced amounts of butyrate, a beneficial gut compound
- An imbalance in gut bacteria may contribute to CFS/ME symptoms like fatigue, brain fog, and digestive issues.
- Test results can guide personalized treatment plans, such as diet changes, probiotics, and therapies to restore gut health.
Next Steps
If you have CFS/ME or suspect gut issues, consider discussing gut microbiome testing with your doctor. Here are some steps:
- Research reputable testing labs and consult your doctor on the best test for you (stool, breath, or blood).
- Follow any dietary or medication guidelines to ensure accurate results.
- Work with your healthcare team to interpret results and develop a tailored treatment plan based on your gut microbiome and CFS/ME symptoms.
- Be prepared to make lifestyle and dietary changes, take probiotics or prebiotics, and explore other therapies as recommended.
- Monitor your progress and adjust your treatment plan as needed, with regular follow-up testing to track changes in your gut microbiome.
FAQs
Can gut troubles lead to constant tiredness?
Yes, recent studies show that imbalances in the gut microbiome (the collection of bacteria in the digestive system) may contribute to chronic fatigue syndrome (CFS/ME). Researchers found lower levels of certain beneficial gut bacteria like Faecalibacterium prausnitzii and Eubacterium rectale in CFS/ME patients. These bacteria produce butyrate, a compound that helps reduce inflammation. A lack of butyrate is linked to bacterial imbalances and fatigue symptoms.
Is chronic fatigue syndrome related to the microbiome?
| Connection | Details |
|---|---|
| Confirmed Link | Multiple studies confirm a significant connection between chronic fatigue syndrome and changes in the gut microbiome composition. |
| Reduced Diversity | CFS/ME patients tend to have lower diversity of gut bacteria compared to healthy individuals. |
| Bacterial Imbalance | Those with CFS/ME often have lower levels of anti-inflammatory bacteria and higher levels of pro-inflammatory bacteria. |
| Structural Differences | The overall structure and similarity of the gut microbiome shows notable differences in people with CFS/ME. |
Related posts
- Probiotics for ME/CFS: Checklist to Get Started
- Top 8 Probiotic Strains for CFS/ME Symptom Relief
- Probiotics for Chronic Fatigue & Gut Health: Benefits
- Homeopathic Remedies for CFS/ME: Treatment Guide





Leave a Reply