Mycotoxins, toxic substances produced by certain molds and fungi, have been linked to Chronic Fatigue Syndrome (CFS). Research shows a staggering 93% of CFS patients tested positive for at least one mycotoxin in their urine, compared to 0% in healthy individuals without mold exposure.
The most prevalent mycotoxins found in CFS patients are:
| Mycotoxin | Prevalence |
|---|---|
| Ochratoxin A (OTA) | 80.9% |
| Gliotoxin | 39.8% |
| Aflatoxin | 29.6% |
Mycotoxin exposure can contribute to CFS symptoms through various mechanisms:
-
Immune system problems
-
Oxidative stress
-
Mitochondrial dysfunction
-
Neurotoxicity
Addressing potential mycotoxin exposure by reducing exposure sources, implementing detoxification strategies, and providing targeted therapeutic interventions may help alleviate symptoms and improve overall well-being in individuals with CFS.
Related video from YouTube
What are Mycotoxins?
Mycotoxins are toxic substances produced by certain types of mold and fungi. They can contaminate food and the environment, posing a risk to human and animal health.
Exposure Sources
We are exposed to mycotoxins through:
-
Dietary Sources: Spoiled or moldy food products, such as grains, nuts, spices, dried fruits, and coffee beans.
-
Environmental Sources: Living or working in water-damaged buildings, exposure to outdoor molds, and airborne dust containing mold spores.
Types of Mycotoxins
Here are some common and harmful mycotoxins:
| Mycotoxin | Produced by | Health Effects |
|---|---|---|
| Aflatoxins | Aspergillus molds | Liver damage, immune suppression, cancer |
| Ochratoxin A | Kidney disease, cancer | |
| Fumonisins | Esophageal cancer, other health issues | |
| Trichothecenes | Inhibits protein synthesis, gastrointestinal issues, immune suppression, internal haemorrhaging | |
| Zearalenone | Disrupts hormonal balance, reproductive problems |
Health Effects
Mycotoxin exposure can cause:
-
Liver and kidney damage
-
Immune system suppression
-
Gastrointestinal distress
-
Reproductive issues
-
Increased cancer risk
The severity of these effects depends on the type and concentration of mycotoxins, as well as the duration of exposure and individual susceptibility.
Understanding Chronic Fatigue Syndrome
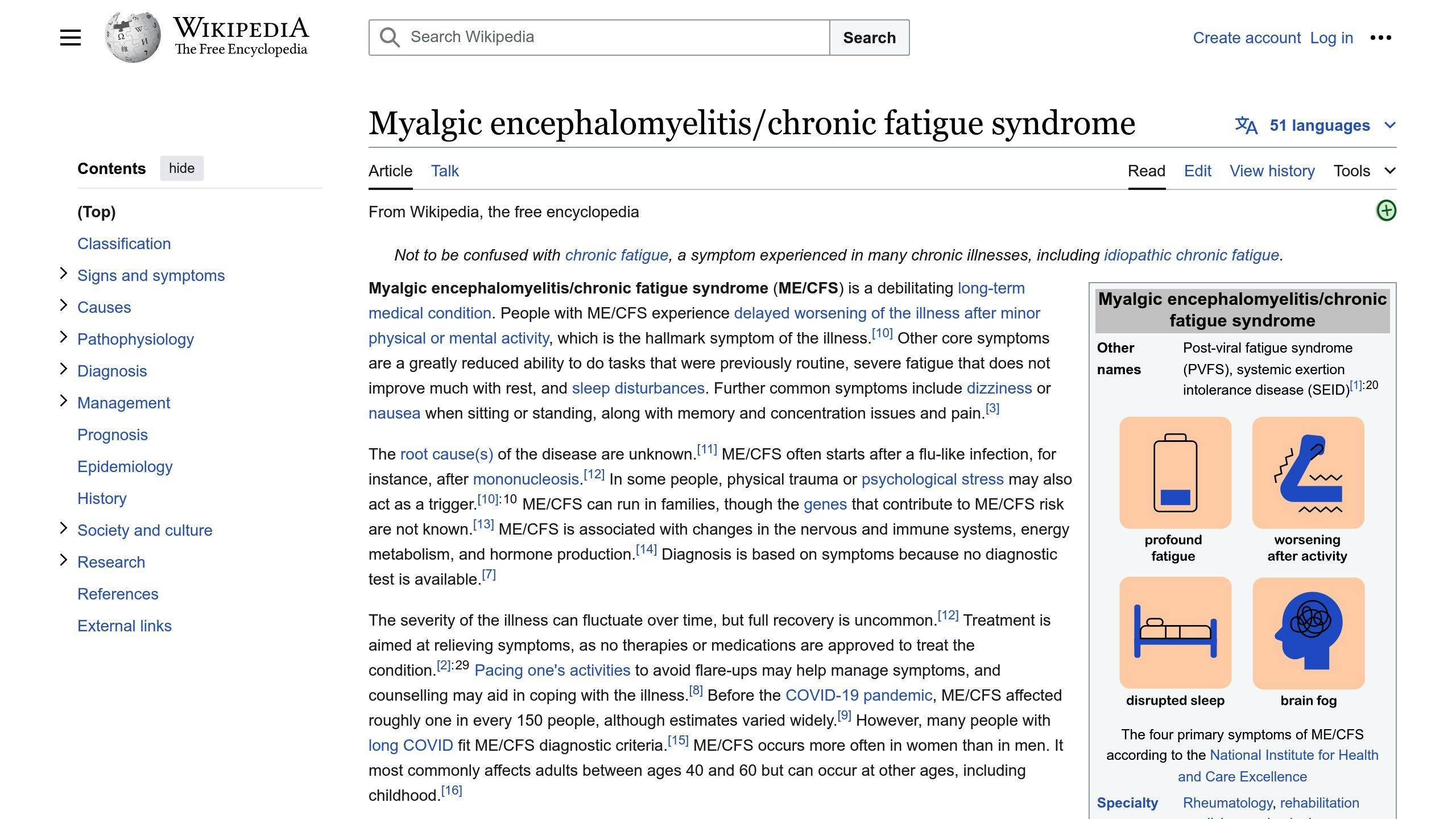
Chronic Fatigue Syndrome (CFS), also known as Myalgic Encephalomyelitis (ME/CFS), is a complex and debilitating disorder. It is characterized by extreme fatigue that lasts for at least six months and is not relieved by rest.
Key Symptoms
In addition to extreme fatigue, ME/CFS often involves:
-
Post-exertional malaise: Symptoms worsen after physical or mental exertion, often delayed by hours or days.
-
Unrefreshing sleep: Waking up feeling unrested, despite adequate rest.
-
Cognitive impairment: Difficulties with concentration, memory, and information processing.
-
Pain: Chronic, widespread muscle and joint pain.
-
Flu-like symptoms: Recurrent sore throat, headaches, and low-grade fever.
-
Sensory sensitivities: Increased sensitivity to light, sound, odors, and certain foods or medications.
Diagnosis and Impact
ME/CFS is diagnosed by ruling out other potential causes of fatigue. The diagnostic process involves evaluating symptoms, physical examination, and various tests.
The impact of ME/CFS on daily life can be significant. The debilitating fatigue and associated symptoms can disrupt daily activities, work, and social interactions, leading to a substantial reduction in overall functioning and well-being.
| Symptom | Description |
|---|---|
| Fatigue | Extreme physical and mental exhaustion |
| Post-exertional malaise | Worsening of symptoms after exertion |
| Unrefreshing sleep | Waking up feeling unrested |
| Cognitive impairment | Difficulties with memory, concentration, and information processing |
| Pain | Chronic, widespread muscle and joint pain |
| Flu-like symptoms | Recurrent sore throat, headaches, and low-grade fever |
| Sensory sensitivities | Increased sensitivity to light, sound, odors, and certain substances |
ME/CFS is a complex condition that significantly affects daily functioning and overall quality of life. Understanding the symptoms and diagnostic process is crucial for proper management and support.
1. Mycotoxins
Prevalence in Patients
Mycotoxins are common in many environments and can contaminate various food sources, increasing the risk of exposure for individuals with Chronic Fatigue Syndrome (CFS). While the exact prevalence of mycotoxin exposure in CFS patients is not well-documented, some studies suggest a potential link:
-
A study by Brewer et al. (2013) found that 93.5% of CFS patients tested positive for mycotoxins in their urine samples, indicating widespread exposure.
-
Research by Shoemaker et al. (2010) reported that CFS patients had significantly higher levels of certain mycotoxins (ochratoxin A and macrocyclic trichothecenes) compared to healthy controls.
Potential Contribution to CFS
While the exact role of mycotoxins in the development or exacerbation of CFS is not fully understood, several mechanisms have been proposed:
-
Immune system problems: Mycotoxins can suppress or overstimulate the immune system, potentially contributing to the immune dysfunction observed in CFS patients.
-
Oxidative stress: Exposure to mycotoxins can increase oxidative stress, which has been linked to fatigue and other CFS symptoms.
-
Mitochondrial problems: Some mycotoxins may impair mitochondrial function, leading to energy deficits and fatigue.
-
Neurotoxicity: Certain mycotoxins can cross the blood-brain barrier and potentially contribute to neurological symptoms associated with CFS.
Detection Methods
Detecting mycotoxin exposure in CFS patients can be challenging due to the variety of mycotoxins and their metabolites. Common methods include:
| Detection Method | Description |
|---|---|
| Urine analysis | Testing for the presence of mycotoxins or their metabolites in urine samples. |
| Blood analysis | Measuring mycotoxin levels or biomarkers in blood samples. |
| Environmental testing | Assessing potential sources of mycotoxin exposure in the patient’s living or working environment. |
| Immunoassays | Using antibody-based tests to detect specific mycotoxins or their metabolites. |
Health Implications
Chronic exposure to mycotoxins can have various adverse health effects, some of which may overlap with or exacerbate CFS symptoms:
-
Fatigue and weakness
-
Cognitive impairment and brain fog
-
Digestive issues and nausea
-
Headaches and muscle pain
-
Respiratory problems
-
Immune system problems and increased susceptibility to infections
Addressing potential mycotoxin exposure through environmental remediation, dietary changes, and detoxification strategies may help alleviate symptoms and improve overall health in CFS patients.
2. Chronic Fatigue Syndrome
Prevalence in Patients
Chronic Fatigue Syndrome (CFS) affects a significant number of people worldwide. According to estimates, it affects:
| Population | Prevalence |
|---|---|
| General population | 0.2% to 2.5% |
| Women | Higher prevalence than men |
The exact prevalence of CFS can be difficult to determine due to the complexity of diagnosing the condition and the lack of a single confirmatory test.
Potential Contribution to CFS
The exact cause of CFS is unknown, but it is believed to involve a combination of factors, including:
-
Viral infections
-
Immune system dysfunction
-
Hormonal imbalances
-
Environmental exposures
Some research suggests that exposure to mycotoxins may contribute to the development or exacerbation of CFS through various mechanisms, including:
-
Immune system dysregulation
-
Increased oxidative stress
-
Mitochondrial dysfunction
-
Neurotoxicity
Addressing potential mycotoxin exposure, if present, may help alleviate some of the symptoms associated with CFS and improve overall health and well-being.
sbb-itb-cf04d29
Comparing Mycotoxin Prevalence
The presence of mycotoxins in patients with Chronic Fatigue Syndrome (CFS) has been studied extensively. Research suggests that CFS patients are more likely to have mycotoxins in their systems compared to the general population.
Prevalence Comparison Table
| Population | Mycotoxin Prevalence |
|---|---|
| CFS Patients | 93% tested positive for at least one mycotoxin |
| General Population (No Mold Exposure) | 0% tested positive for mycotoxins |
A study by Brewer et al. (2013) found that 93% of CFS patients (104 out of 112) had at least one mycotoxin present in their urine samples. In contrast, a control group of healthy individuals with no history of mold exposure (n=55) showed no positive cases of mycotoxins.
The study also revealed that approximately 30% of the CFS patients had more than one mycotoxin present in their urine. Ochratoxin A (OTA) was the most common mycotoxin, detected in 83% of the patients, followed by macrocyclic trichothecenes (MT) at 44%.
These findings suggest a potential link between mycotoxin exposure and the development or exacerbation of CFS. The significantly higher prevalence of mycotoxins in CFS patients compared to the general population highlights the importance of considering mycotoxin exposure as a potential contributing factor in the etiology of CFS.
Evaluating Mycotoxins’ Contribution to CFS
Research has investigated the potential role of mycotoxins in contributing to the development or exacerbation of Chronic Fatigue Syndrome (CFS). While the exact mechanisms are not fully understood, the evidence suggests that mycotoxin exposure may be a significant contributing factor in some cases of CFS.
Contribution Comparison Table
| Study | Evidence of Mycotoxin Contribution | Proposed Mechanisms |
|---|---|---|
| Brewer et al. (2013) | Strong evidence: 93% of CFS patients had mycotoxins in urine, compared to 0% in healthy controls. | Mycotoxins can cause oxidative stress, inflammation, and immune dysregulation, which are implicated in CFS pathogenesis. |
| Tuuminen and Rinne (2014) | Moderate evidence: Mold hypersensitivity linked to CFS and multiple chemical sensitivity. Mold exposure may trigger CFS in susceptible individuals. | Immune activation and inflammation in response to mold/mycotoxin exposure could lead to CFS symptoms. |
| Hooper et al. (2009) | Suggestive evidence: Mycotoxin exposure associated with fatigue, cognitive impairment, and other CFS-like symptoms. | Mycotoxins can disrupt mitochondrial function, leading to fatigue and other symptoms. |
| Craner (2018) | Supportive evidence: Case studies of CFS patients improving after reducing mycotoxin exposure and implementing detoxification strategies. | Mycotoxins may contribute to a chronic inflammatory state, which can be alleviated by reducing exposure and supporting detoxification pathways. |
The evidence suggests that mycotoxin exposure may contribute to CFS symptoms through various biological mechanisms. Reducing mycotoxin exposure and supporting detoxification pathways may potentially alleviate symptoms in some CFS patients.
Comparing Mycotoxin Detection Methods
Detecting mycotoxins in biological samples is crucial for understanding their potential role in Chronic Fatigue Syndrome (CFS). Various analytical methods have been employed, each with its own strengths and limitations.
Detection Methods Comparison Table
| Method | Sensitivity | Specificity | Practicality |
|---|---|---|---|
| Enzyme-Linked Immunosorbent Assay (ELISA) | Moderate to high | Moderate | Rapid, cost-effective, suitable for screening |
| Liquid Chromatography-Mass Spectrometry (LC-MS/MS) | High | High | Accurate, can detect multiple mycotoxins simultaneously, requires specialized equipment and expertise |
| Immunoaffinity Columns | Moderate to high | High | Effective sample clean-up, can be combined with LC-MS/MS for improved sensitivity and specificity |
| Polymerase Chain Reaction (PCR) | Moderate | High | Detects mycotoxin-producing fungi, indirect measure of mycotoxin presence |
The choice of detection method depends on factors such as the desired sensitivity and specificity, sample throughput, and available resources. ELISA is widely used for initial screening due to its simplicity and cost-effectiveness, while LC-MS/MS offers higher sensitivity and specificity for confirmatory analysis. Immunoaffinity columns can enhance the detection capabilities of LC-MS/MS by reducing matrix interference. PCR-based methods can complement chemical analysis by identifying the presence of mycotoxin-producing fungi.
In the context of CFS research, a combination of screening and confirmatory methods may be necessary to accurately assess mycotoxin exposure levels and their potential contribution to the condition. Ongoing advancements in analytical techniques continue to improve the detection and quantification of mycotoxins in biological samples.
Health Implications of Mycotoxins in CFS
Mycotoxins can have serious health effects, especially for people with Chronic Fatigue Syndrome (CFS). Understanding these health implications is crucial for developing effective management strategies and improving patient outcomes.
Health Implications of Mycotoxins
| Health Issue | Description | Potential Therapeutic Approach |
|---|---|---|
| Immune System Problems | Mycotoxins can disrupt the immune system, leading to chronic inflammation and autoimmune responses. | Immunomodulatory therapies, such as low-dose naltrexone or anti-inflammatory agents, may help regulate the immune system and alleviate symptoms. |
| Oxidative Stress | Mycotoxin exposure can cause oxidative stress, damaging cells and tissues, and exacerbating fatigue and cognitive impairment in CFS patients. | Antioxidant supplementation, such as vitamin C, vitamin E, and glutathione, may help counteract oxidative stress and support cellular function. |
| Mitochondrial Dysfunction | Mycotoxins can disrupt mitochondrial function, leading to impaired energy production and increased fatigue. | Mitochondrial support therapies, such as coenzyme Q10, L-carnitine, and D-ribose, may help improve energy production and alleviate fatigue. |
| Neurotoxicity | Certain mycotoxins, like ochratoxin A, can cross the blood-brain barrier and exert neurotoxic effects, potentially contributing to cognitive impairment and neurological symptoms in CFS patients. | Neuroprotective agents, such as alpha-lipoic acid and curcumin, may help mitigate the neurotoxic effects of mycotoxins and support cognitive function. |
| Detoxification Support | The body’s ability to eliminate mycotoxins may be compromised in CFS patients, leading to accumulation and prolonged exposure. | Strategies to support detoxification pathways, such as glutathione precursors, binders, and chelators, may help facilitate the removal of mycotoxins from the body. |
Addressing these potential health implications through targeted therapeutic interventions may help alleviate symptoms and improve overall well-being in individuals with CFS. It is essential to work closely with healthcare professionals to develop an individualized treatment plan based on the patient’s specific needs and circumstances.
Conclusion
The connection between mycotoxins and Chronic Fatigue Syndrome (CFS) is a significant one. Research has shown that mycotoxins, particularly ochratoxin A (OTA), are commonly found in the urine samples of CFS patients. In some studies, detection rates were as high as 93%.
Mycotoxins can have serious health effects, including immune system problems, oxidative stress, mitochondrial dysfunction, and neurotoxicity. These effects are consistent with the symptoms experienced by CFS patients.
While the exact mechanisms behind the potential role of mycotoxins in CFS are not yet fully understood, the available evidence suggests that environmental exposures, particularly to water-damaged buildings and mold, may be contributing factors to this condition.
Future Research Directions
To better understand the connection between mycotoxins and CFS, further research is needed. This includes:
| Research Direction | Description |
|---|---|
| Large-scale studies | Conducting larger studies with robust control groups and standardized methodologies for mycotoxin detection and quantification. |
| Mechanisms of mycotoxin effects | Exploring the specific mechanisms by which different mycotoxins contribute to the development and perpetuation of CFS symptoms. |
| Synergistic effects | Investigating the potential synergistic effects of multiple mycotoxin exposures, as well as the interplay with other environmental and genetic factors. |
| Therapeutic interventions | Evaluating the efficacy of various therapeutic interventions, such as detoxification strategies, immunomodulatory agents, and mitochondrial support, in alleviating mycotoxin-related health effects in CFS patients. |
By addressing these research gaps, we can gain a deeper understanding of the role of mycotoxins in CFS and potentially develop more effective prevention, diagnosis, and management strategies for this complex condition.
FAQs
What are the mycotoxins in CFS?
The most common mycotoxins found in the urine of ME/CFS patients with a history of chronic mold exposure are:
| Mycotoxin | Prevalence |
|---|---|
| Ochratoxin A (OTA) | 80.9% |
| Gliotoxin | 39.8% |
| Aflatoxin | 29.6% |
OTA was the most frequently detected mycotoxin, present in over 80% of the ME/CFS patients studied. Gliotoxin and aflatoxin were also found in a significant proportion of patients, suggesting that exposure to multiple mycotoxins may contribute to the development or exacerbation of CFS symptoms.
Read about other perceived causes of CFS
Related posts
- Antioxidants for CFS/ME: Benefits, Diet Tips
- Probiotics Improve Cognitive Function in ME/CFS
- Anti-Inflammatory Diet for CFS/ME: Foods to Eat & Avoid
- Food Sensitivities, Intolerances & Gut Health in CFS/ME





Leave a Reply